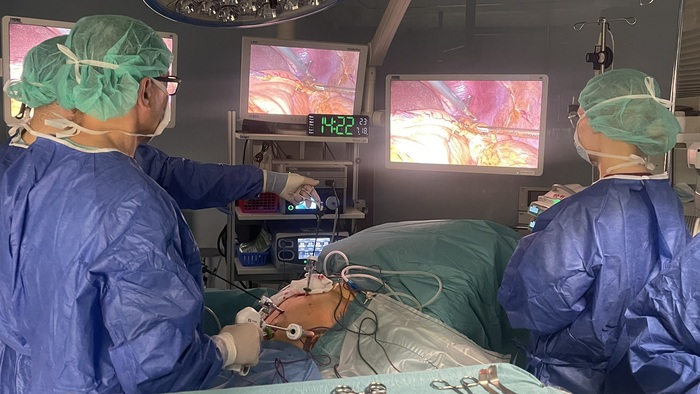
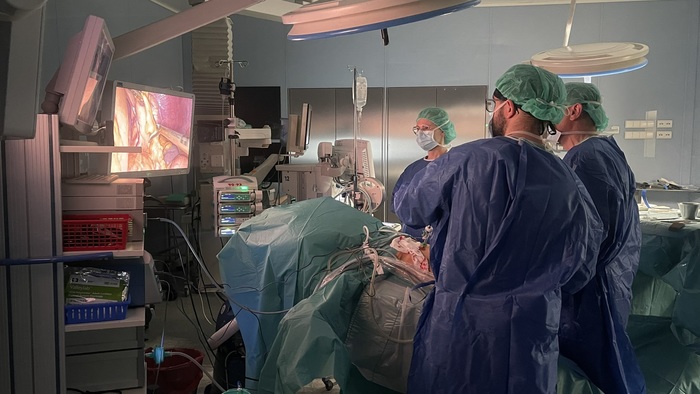
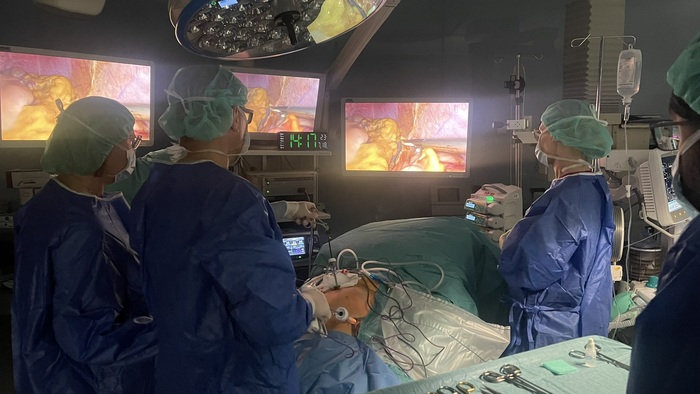
Medical University of Gdańsk hospital introduces minimally invasive laparoscopic distal pancreatectomy
25.09.2025
The University Clinical Centre in Gdańsk, the MUG hospital, has introduced a minimally invasive laparoscopic technique for distal pancreatectomy. Until recently, this procedure was performed primarily using the traditional open method, requiring a large surgical incision.
We have adopted this modern treatment approach mainly for conditions operated on before malignant transformation occurs – primarily cystic tumours and small neuroendocrine tumours,” explains Assoc. Prof. Stanisław Hać, M.D., Ph.D., D.Sc., from Department of Surgical Oncology, Transplant Surgery and General Surgery at the Medical University of Gdańsk.
Distal pancreatectomy involves the removal of a portion of the pancreas, usually the tail or body, to treat malignant or pre-malignant lesions. At UCC, this procedure, previously performed routinely with a wide incision, is now increasingly carried out in a minimally invasive manner using laparoscopic access.
We perform the procedure whenever it is technically feasible and does not require extending the surgery due to the necessity of removing structures surrounding the pancreas, adds Prof. Hać.
One of the key advantages of minimally invasive distal pancreatectomy is that the pancreas is not disconnected from the gastrointestinal tract.
After transecting the pancreas transversely, the cut site is secured without the need for anastomosis. This makes the surgery simpler and shorter, emphasises the surgeon. For patients, it means significantly less physical strain and greater comfort – reduced trauma, less pain, and a lower risk of wound-healing complications, as the incision is much smaller. Recovery is faster, including earlier return to physical activity. Importantly, oncological outcomes and treatment effectiveness remain identical to those of the traditional method.”
According to the specialists, eligibility for the minimally invasive approach depends on individual patient characteristics. Notably, age is not one of the exclusion criteria.
Cardiovascular conditions may pose a risk of pneumoperitoneum, in which case one must carefully assess whether the benefits of reduced surgical trauma outweigh cardiovascular risks. There are also technical considerations, such as previous surgeries or adhesions in the area, which would more likely indicate a preference for the traditional method, notes Prof. Hać.
At present, laparoscopic distal pancreatectomy at the UCC is performed mainly in patients diagnosed with conditions carrying a high risk of malignant transformation.
These are primarily cystic tumours and small neuroendocrine tumours, says Prof. Hać. As our surgical team gains more experience, we plan to expand the indications and gradually increase the number of such procedures.
To date, several laparoscopic distal pancreatectomies have already been performed with very good clinical outcomes.
All patients have fully recovered, and complications typical for this type of surgery occurred with similar frequency as in the traditional method and were successfully managed.
Minimally invasive procedures are reimbursed by the National Health Fund and are available to patients as part of standard medical care. The introduction of modern surgical techniques marks another step by the University Clinical Centre toward improving patient safety and comfort during and after surgery, while also raising treatment standards.
photo: Łukasz Wojtowicz/UCK
Archives
- Academic Year 2024/2025
- Academic Year 2023/2024
- Academic Year 2022/2023
- Academic Year 2021/2022
- Academic Year 2020/2021
- Academic Year 2019/2020
- Academic Year 2018/2019
- Academic Year 2017/2018
- Academic Year 2016/2017
- Academic Year 2015/2016
- Academic Year 2014/2015
- Academic Year 2013/2014
- Academic Year 2012/2013